California’s ObamaCare exchange is announcing a cap on patients’ costs for high-priced specialty drugs, the first state in the country to do so.
The announcement, which comes after a unanimous vote by the exchange’s board Thursday, would cap the cost for most enrollees on the insurance exchange at $250 per prescription per month.
Under the current system, enrollees have to pay costs up to the deductible on their plan, which can be thousands of dollars.
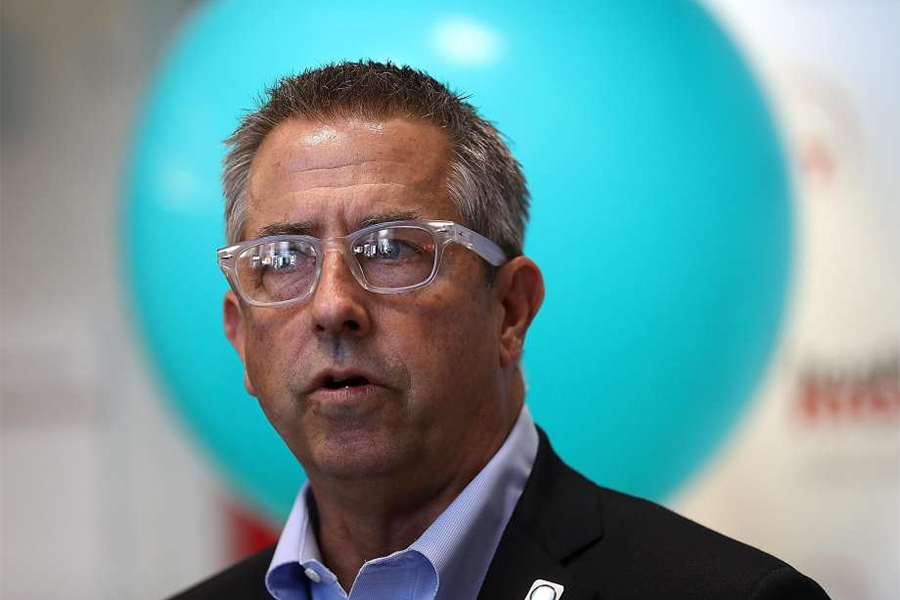
“This is the first time that an exchange has ensured that all of its consumers have access to the medications they need,” said the exchange’s executive director, Peter Lee.
Advocates hope California’s action will spur other states to enact caps as well.
The move comes amid increasing scrutiny of new high-priced drugs. For example, a new treatment for Hepatitis C called Sovaldi can cost $84,000 for a 12-week treatment.
California’s move caps the cost for patients, but it does not change the high prices, which have to be picked up by insurers.
Insurers have been putting pressure on drug companies over high prices.
A March report from Express Scripts, the largest U.S. manager of prescription benefits, found that specialty drugs like Sovaldi drove a 13 percent increase in U.S. prescription drug spending last year, the largest increase since 2003.
“While Covered California is doing its part to protect consumers against these rising costs, a broader solution is needed to curtail the explosion in specialty drug costs so that consumers get the care they need without driving up insurance costs so much that consumers can no longer afford coverage,” Lee said.
Original article published by Peter Sullivan of The Hill on May 22, 2015.