Up to 50% of people who are hospitalized are either malnourished or at risk for malnutrition. Being in a state of malnutrition can cause delayed wound healing, infection and other problems than may lead to hospital readmissions.
September 28th through October 2nd, 2015
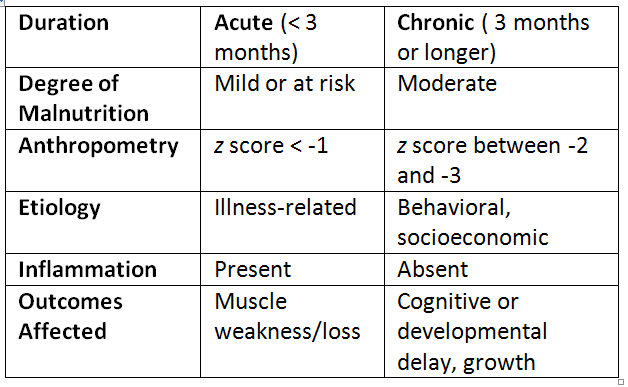
What is malnutrition?
There is currently no clear definition of malnutrition in terms of diagnosis but a set of characteristics has been proposed by the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) and the Academy of Nutrition and Dietetics (AND):
| Malnutrition Syndrome | Level of inflammation | Associated Conditions |
| Starvation-related | None | Anorexia nervosa |
|
Chronic disease-related |
Mild to moderate | Organ failure, cancer, rheumatoid arthritis |
| Acute disease-related | Severe | Major infection, burns, trauma or closed head injury |
Consequences of Malnutrition
Malnourished patients are:
- 2 to 3 times more likely to have post-operative complications, such as infection and delayed wound healing.
- 2 times as likely to require specialized care at home.
- More frequently admitted to the hospital and have longer hospital stays.
Recognizing Malnutrition
Some of the signs of malnutrition include:
- Unplanned weight loss
- Loss of appetite
- Not eating or only eating small amounts
- Weakness and/or fatigue
Preventing and Treating Malnutrition
Health care professionals and caregivers can take measures to maintain or improve nutritional status:
- Screen for malnutrition upon admission to the hospital or long term care facility
- Many screening tools are available, including the Mini Nutritional Assessment (MNA®)
- Refer to a Registered Dietitian Nutritionist for preventive care and treatment.
- Consider oral nutrition supplements (ONS) to supplement poor oral intake
- ONS have been shown to reduce hospital length of stay, 30-day hospital readmission and total health care costs.
- Have a post-discharge nutrition plan
- Provide a ONS prescription or recommendation if needed.
- Collaborate with a Registered Dietitian Nutritionist.
- Arrange for follow-up medical care.
Caregiver Tips
Elderly caregivers are at particular risk for malnutrition. In a study of 76 family caregivers (mean age 70 years) who spent an average of 100 hours per week on caregiving activities:
- 13% reported not eating
- 21% were at risk for malnutrition
A decrease in overall food intake makes nutrient-dense foods even more important for older adult caregivers. Keep healthy foods on hand, such as:
- Low-fat yogurt and milk
- Whole grain bread/crackers/tortillas
- Beans, eggs, cheese
- Nuts, seeds, nut butters
- Brightly-colored fruits and vegetables
- Water, milk and other fluids
Reference
- Making Optimal Nutrition a National Standard (A.S.P.E.N. Clinical Nutrition Webinar Series)
- Malnutrition Awareness: Bringing it to the Masses (A.S.P.E.N. Clinical Nutrition Webinar Series)
- Torres SJ, et al. Depression, nutritional risk and eating behaviour in older caregivers. J Nutr Health Aging. 2010;14(6):442-8