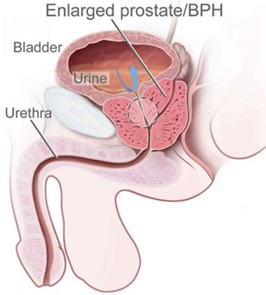
The prostate is a small gland in men – and in people assigned male at birth (AMAB) – that is nestled just beneath the bladder. It is about the size of a ping pong ball and consists of connective tissues and glandular tissues. The primary purpose of the prostate gland is to produce seminal fluid that mixes with sperm, making up a portion of semen. This seminal fluid helps protect the genetic material contained in the sperm, along with serving other functions. The prostate also contains smooth muscles that help with ejaculation.
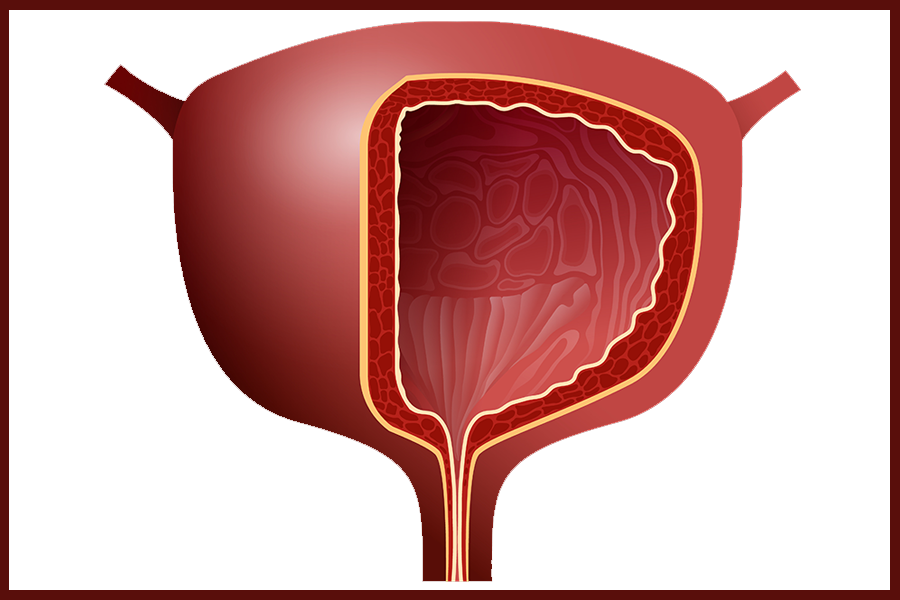
Benign prostatic hyperplasia (BPH), or an enlarged prostate, is a common health issue in men and people assigned male at birth. The prostate typically grows larger with age. As it becomes enlarged, it can put pressure on the bladder and the urethra. Because the urethra runs directly through the prostate, an enlarged prostate can squeeze the urethra and cause problems in passing urine. Urinary problems can begin in middle age, or they may not be noticed until later in life.
The impact of an enlarged prostate varies widely. For some, it is an occasional annoyance. For others, it can interfere with bladder function, leading to complications with emptying the bladder or causing a frequent need to urinate. In some cases it requires surgery.
Changes in the Prostate with Age
In a typical male, the prostate changes with age as follows:
Prostate in Youth
In childhood, the prostate is small and composed mostly of fibromuscular stroma and rudiments of ducts.
Prostate at Puberty
With the influx of hormones during puberty, the prostate increases in size. There is a proliferation of prostatic follicles (gland tissue).
Prostate in the 3rd Decade
Around the third decade of life, the prostate may develop atypical epithelial infoldings in the lumen of the follicles.
Prostate in the 4th Decade
Approaching middle age, the typical prostate stays a fairly continuous size. The epithelial infoldings slowly vanish, and amyloid concretions appear in the follicles.
Prostate in the 5th Decade and Onward
From the fifth decade onward, some measure of prostatic hypertrophy (enlargement of the prostate gland) is usually present. In some cases the gland reduces in size instead (atrophies), which is called senile atrophy.
What Causes an Enlarged Prostate?
It’s not exactly clear what the reason is behind an enlarged prostate, though the prostate continues to grow throughout a person’s life. There is some association with obesity, genetics, erectile dysfunction, type 2 diabetes and overall poor health.
When the prostate gland is enlarged and the cause is not cancer or inflammation, it is referred to as “benign prostatic hyperplasia” (BHP). But BHP can exist concurrently with other conditions such as cancer. It is important to visit your doctor or urologist to confirm your diagnosis if you suspect an enlarged prostate. Your doctor will run tests to rule out other problems. If it does turn out you have a benign prostatic hyperplasia (BHP), know that you’re not alone! About one-third of men, as well as people assigned male at birth, experience moderate to severe symptoms of BHP by age 60. About half do so by age 80.
Testing for Benign Prostatic Hyperplasia (BHP)
Your doctor may recommend several tests to identify if you have benign prostatic hyperplasia. These tests may include a digital rectal exam also known as a prostate exam, a prostate MRI scan, a urine test and a blood test (PSA). The rectal exam will confirm that your prostate is enlarged. The urine test can check for an infection that could cause inflammation. And the blood test can check for issues with your kidneys and provide early signs of prostate cancer.
Your doctor will also ask you about any symptoms you are experiencing. Symptoms of BHP may include:
- A weak or interrupted urinary stream
- Sudden urgency to urinate
- Frequent urination
- Inability to completely empty the bladder during urination
- Trouble initiating urine flow even when bladder feels full
- Intermittency: the need to stop and start several times when passing urine
- Nocturia: the need to wake up at night more than two times to pass urine
Reasons to visit the doctor
If you suspect your prostate is enlarged, make an appointment with your doctor right away.
It is time to visit your doctor if you are:
- Having difficulty urinating and/or needing to pee more frequently during the day.
- Waking up more than twice per night to pee.
- Having trouble with starting to urinate.
- Dribbling at the end of urination.
- Experiencing a weaker than usual urine stream, or finding it easier to urinate while sitting down.
- Experiencing bladder infections or seeing blood in your urine
If you discover you have no ability to urinate at all, seek emergency medical treatment right away. Acute urinary retention can cause severe pain and be life-threatening.
But What If It’s Cancer?
Fears about a cancer diagnosis prevent many individuals from visiting the doctor. However – like many health issues – the sooner it is identified, the more treatment options you have and the better your chances of survival. Fortunately, low-risk prostate cancer often grows very slowly, or it doesn’t grow at all. In many individuals diagnosed with prostate cancer, the cancer cells grow so slowly that they never break free of the gland. Because of this, a treatment approach known as “active surveillance” can be considered as an alternative to radiotherapy or surgery.
Coudé Tip Catheters
If your prostate is enlarged, or if you’ve had treatment for prostate cancer, you may need a urinary catheter to fully drain your bladder. Catheters are designed with straight tips for straightforward insertion, and with coudé tips to help navigate obstacles.
The coudé-tipped catheter is a catheter with a curved tip. It is used when an individual has an enlarged prostate gland or there is an obstruction in the urethra that a normal straight tipped catheter cannot circumvent. If your physician orders a coudé-tipped catheter for you, he/she must write “coudé tip catheter” on the prescription and document the reason. These reasons may include anatomical obtructions, or a Koch or Indiana pouch. Coudé-tipped catheters are not something you can request without a prescription.
Sources include:
- “Benign Prostatic Hyperplasia” webinar, presented by Kelly Sparks, RN, BSN, WOCN, CFCN with Capital Nursing Education
- National Institute on Aging
- Clevelandclinic.org
Illustrations provided by Kelly Sparks at Capital Nursing Education (https://healthjade.net/wp-content/uploads/2019/07/benign-prostatic-hypertrophy.jpg)