End of life decisions are hard to make, for yourself or for a loved one. They may include treatment and medication choices, and if and when to provide artificial means of nutrition or hydration.
When someone stops eating enough, it can be tremendously difficult on the family and or caregiver. Food and nourishment are how we show love. We don’t want anyone to “starve”. We want to nourish, feed, and protect.
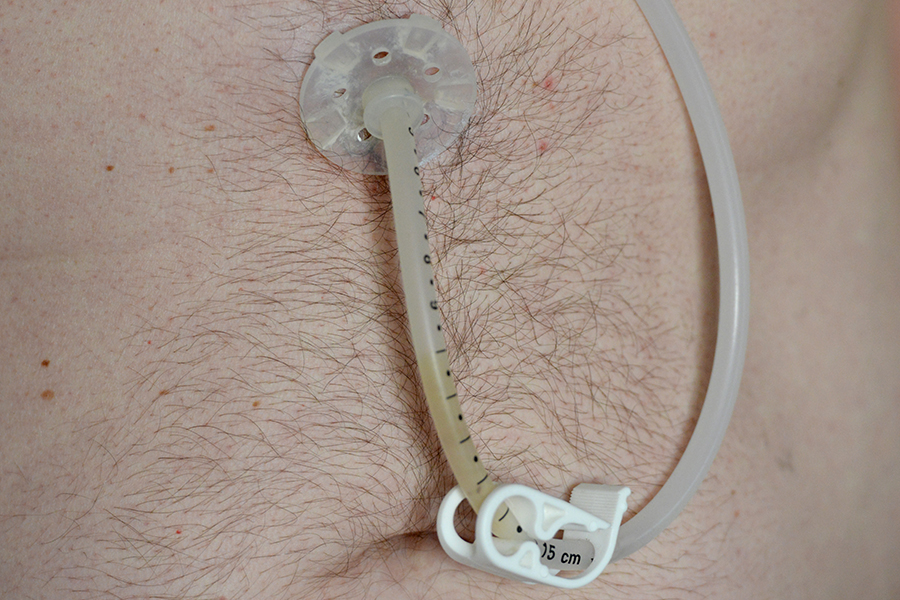
But when someone is dying, they eat less and less. Determining if and when a patient has a feeding tube inserted is a complicated and oftentimes emotionally-charged decision.
Having that conversation BEFORE a patient becomes terminally ill will help reduce the stress and strain the decision may cause.
As the Caregiver
- Has your loved one ever spoken about what s/he wants at the end of their life? Specifically if they would want a feeding tube?
- What are your loved one’s beliefs? Does their faith play a role in this decision?
- How to they want to spend their last days? What does that “look” like for them?
Another good way to make a decision is to ask the doctors questions such as:
- Will being fed via a feeding tube extend his/her life?
- Will it make them more comfortable?
- Will the feeding tube change the way s/he lives his or her life?
- Are there any side effects?
- How long before we can expect results?
- If we don’t insert a feeding tube, what can happen?
As the Patient
Making end-of-life decisions for yourself is something nobody wants to think about; it can be even more difficult to discuss these decisions with someone close to you. When making end of life decisions, make sure you consider the following:
- If you stop breathing, do you want to be resuscitated?
- If you stop eating, do you want a feeding tube inserted?
- Do the people close to you know what you want?
- If you are terminally ill, do you want to stay at home, be hospitalized, or go somewhere else?
Documentation or Advanced Directives
Advanced Directives are written instructions letting your family, proxy, and medical staff know what your decisions are, including your will and healthcare power of attorney. A durable power of attorney for healthcare names a relative or close friend to make decisions for you when you’re not able to. This person is called your proxy. Be sure to sign the durable power of attorney or it will NOT be valid. Also, be sure to select a “back-up” proxy in case the first proxy is not available.
It is important to prepare the Advanced Directives so that your family and the medical staff knows what treatment you’ll accept and what treatment you will refuse. This also makes it clear to your family who you chose to make your healthcare decisions. These forms are available at your local hospital. If you don’t make your decisions clear in this type of documentation, it can make it difficult for a loved one to begin to think about what you would want, and the medical staff will do whatever they can to support you with their medical training.
This is one of the hardest decisions you can make for yourself or a loved one, but planning ahead and speaking to your doctor will help your loved ones, the medical staff and most importantly, you.
Additional Resources and Support
For more information surrounding end-of-life care, the following offers resources and support for both patients and caregivers:
www.nia.nih.gov/health/making-decisions-someone-end-life
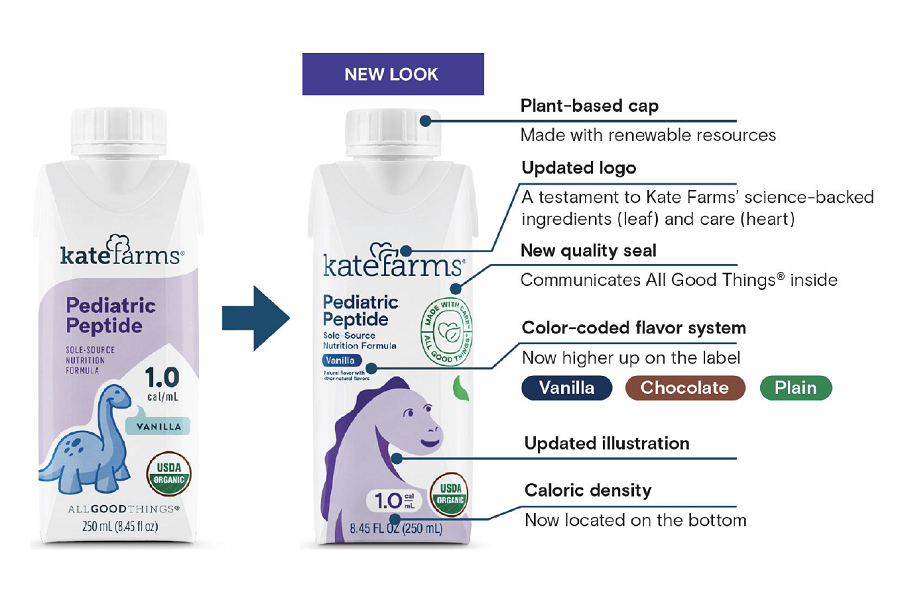
You can also learn more about tube feeding from our free Adult Tube Feeding Guide. This booklet provides the basic information about tube feeding, including how to care for your tube and the skin around it, how to deliver feedings and how to prevent common complications.
Once you enter in your information and click “Submit Request,” you will receive an email with a link to a digital PDF copy of our booklet.