Original article on Helio.com
Clinicians should consider temporary continuous glucose monitoring for any person with diabetes to assess their time spent in the recommended glucose range as an effective guide for treatment decisions, according to a speaker.
HbA1c may underestimate or overestimate a person’s glucose levels, does not reveal glycemic variability and has limited utility for insulin dosing decisions, George Grunberger, MD, FACP, MACE, chairman of the Grunberger Diabetes Institute in Bloomfield Hills, Michigan, said during a presentation at the Heart in Diabetes CME Conference. HbA1c is also unreliable for people with hemolytic anemia and iron deficiency and for those who are pregnant. HbA1c correlation with mean glucose can also vary among racial backgrounds.
“CGM has come of age and is rapidly becoming standard of care, right now, for people with diabetes on intensive insulin regimens,” Grunberger told Healio. “Hopefully, soon it will also become standard for people prescribed any insulin and sulfonylurea therapy — those at risk for hypoglycemia — and eventually replace finger sticking, just as finger sticks superseded urine tests.”
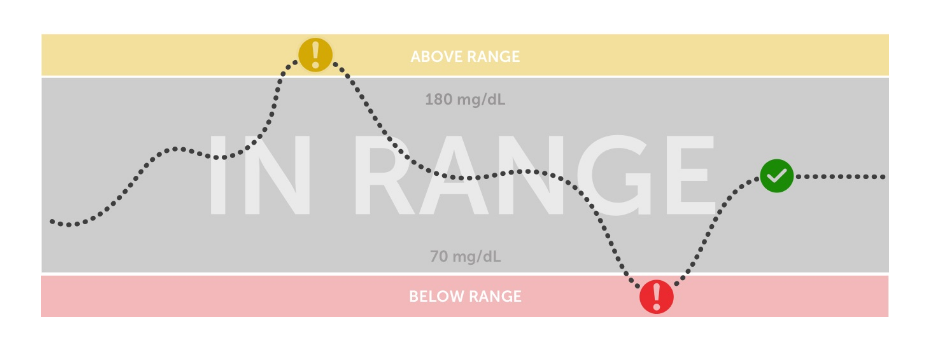
Researchers and clinicians now have a new challenge: to expand the knowledge base for CGM beyond showing increased time spent in the target range — defined as between 70 mg/dL and 180 mg/dL — and minimizing time in hypoglycemia, Grunberger said.
“The challenge is to show improved hard outcomes [with CGM], both in terms of micro- and macrovascular complications of diabetes,” Grunberger told Healio. “This is necessary to justify the use of technology and especially for reimbursement by payers.”
Greater time in range; fewer complications
Data from many studies show that a higher HbA1c is associated increased risk for CV complications and CV mortality, yet the measurement has proven unreliable, Grunberger said.
“The problem is that HbA1c is a strange animal,” Grunberger said during his presentation. “People like it … but if you look at three patients with the same HbA1c of 8%, and then look at their CGM profiles, you will see clearly that they are very different.”
Time in range emerged as a prominent theme among diabetes experts as early as 2016, when the American Association of Clinical Endocrinology convened a consensus conference on CGM to determine new standard simple metrics that could inform therapy adjustment and “get away from HbA1c culture,” Grunberger said.
Ten to 14 days of CGM data, with about 100 glucose readings per day, are necessary to build a “decent” daily profile and inform diabetes management decisions.
“The duration and the number of points have to be there to have something to work with,” Grunberger said.
In one of the first studies to assess risk for diabetes outcomes associated with time in range, published in Diabetes Care in 2018, researchers assessed time in range among hospitalized patients with type 2 diabetes using blinded CGM. Those in the highest quartile, defined as time in range of at least 86%, had the lowest incidence of mild, moderate or vision-threatening diabetic retinopathy.
“That was the first glimpse that maybe time in range can be associated with some diabetes-specific complications,” Grunberger said.
In a study published in Diabetes Care in 2019, researchers evaluated the associations of time in range with development or progression of retinopathy and microalbuminuria using the Diabetes Control and Complications Trial data set — calculating time in range from finger sticks —to validate its use as an outcome measure. In that study, researchers found time in range was “strongly associated” with the risk for microvascular complications and should be an acceptable endpoint for clinical trials.
“Every 10% drop in time in range was associated with a 64% increased risk for retinopathy; likewise for every 10% drop in time in range, there was a 40% increased risk for albuminuria.”
Data also show time in range is associated with prevalence of carotid intima media thickness, CV mortality, and peripheral nerve function in type 2 diabetes.
Potential cost savings
An analysis from the IQVIA Core Diabetes Model showed the potential cost savings of $6.7 billion to $9.7 billion over 10 years if time in range improved from the current average of 58% to 70% or 80% for people with type 1 and type 2 diabetes, when also factoring in the reduction in hypoglycemia.
“Most think of CGM in terms of added cost, but few think in terms of projected potential cost savings,” Grunberger told Healio.
References:
Beck RW, et al. Diabetes Care. 2019;doi:10.2337/dc18-1444.
Lu J, et al. Diabetes Care. 2018;doi:10.2337/dc18-1131.