Blood glucose monitoring (BGM) and continuous glucose monitoring (CGM) can both play a pivotal role in managing diabetes, providing individuals with the tools to track and regulate their glucose levels. While both methods share the common goal of maintaining glycemic control, there are notable differences in their approaches and accuracy.
You can watch an informative video from Dexcom, explaining the difference here.
Blood Glucose Monitoring
Traditional blood glucose monitoring involves periodic testing using a glucose meter and test strips, typically before meals. Individuals prick their fingers to obtain a small blood sample, which is then applied to a test strip for analysis. This method provides a snapshot of blood sugar levels at that specific moment.
Pros:
- Availability: BGM does not require a prescription and is readily available at local pharmacies.
- Accuracy: Blood glucose meters provide the most accurate glucose measurements at a specific moment in time. However, results can easily be skewed if test strips are stored improperly or if the hands are not completely clean, sanitized, and dry before testing.
Cons:
- Painful Fingersticks: The fingertips have the highest concentration of nerve endings in the body. Some discomfort is expected when making a puncture that produces a drop of blood and older individuals may experience difficulty collecting the minimum amount of blood required to perform a test due to poor circulation.
- Inconvenience: Checking levels with a BGM is a process and requires many supplies such as a meter, test strips, lancets, a lancing device, and a control solution. This can be a barrier for some to test regularly, especially while in a public setting.
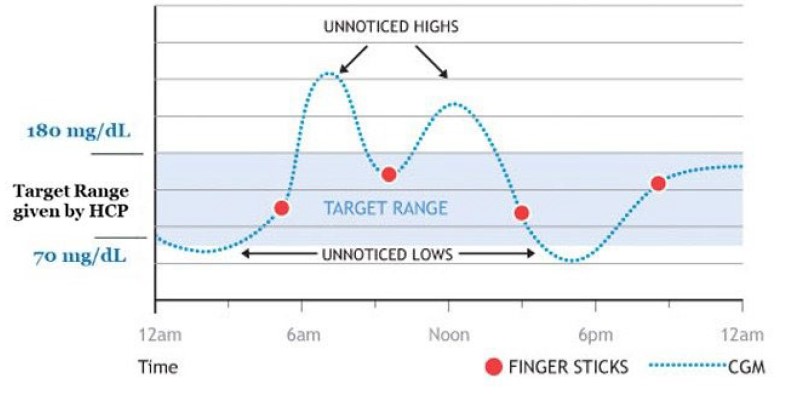
- Unnoticed Highs and Lows: The most compliant individuals will perform a BGM test up to 4 times daily. This, however, is rare as studies suggest 7 out of 10 individuals do not adhere to their prescribed BGM testing regimen. As a result, episodes of high and low glucose go unnoticed and lead to long-term complications such as nerve damage, vision loss, kidney disease, and slow-healing wounds that may lead to lower limb amputations.
Continuous Glucose Monitoring
CGM provides a real-time, continuous stream of data regarding glucose levels. This technology consists of a small sensor inserted under the skin that measures glucose levels in the interstitial fluid, the body fluid between blood vessels and cells. The sensor sends this information wirelessly to a monitoring device or smartphone, allowing for constant tracking 24 hours a day.
Pros:
- No More Fingersticks: While BGM is accurate and reliable in a clinical setting, CGM is more practical for daily self-monitoring. Plus therapeutic CGM systems like FreeStyle Libre 2 and Dexcom G7 are so accurate that the FDA cleared these models for insulin dosing without fingersticks.
- Discreet All-Day Monitoring: Real-time CGM systems provide all-day automatic glucose readings in regular intervals (i.e., every 5 minutes). Data collected by a CGM sensor is equivalent to 288 daily fingersticks without the pain and the hassle.
- Time-in-Range (TIR): TIR is the percentage of time spent in the target glucose range. This range is set by the treating practitioner and varies by individual. More time spent in range is clinically proven to help lower A1C.
- Alerts: CGM sensors provide audible and haptic alerts when glucose levels rise or drop to unsafe levels so individuals can take immediate action. Some CGM systems even provide a 20-minute advanced warning before glucose reaches a critical low level to help avoid a potential hypoglycemic event.
Cons:
- Training: The user will require some training on how to use the device effectively.
- Constantly in Place: The user must wear a sensor on their body (typically on the back of their arm) at all times.
Is BGM or CGM More Accurate?
While BGM is more precise than CGM, it has a greater potential for human error and non-adherence. Additionally, since BGM is usually measured 0-4 times daily, episodes of high and low glucose often go unnoticed. Due to the continuous recording of levels from CGM, it is widely deemed more accurate, providing a wealth of data points for a more precise representation of glucose dynamics.
Take a look at the graph below. Someone who takes fingerstick BGM readings (the red dots) may miss lows and highs if they don’t fall perfectly at the time of testing. CGM is continually checking glucose (the blue dots) throughout the day and night, so the user won’t miss any lows or highs.
Why BGM and CGM readings are sometimes different
When comparing a glucose measurement from a blood glucose meter against a continuous glucose meter, it may be noted that readings are not always identical. One of the main reasons the two may differ is that a BGM measures glucose in the blood, while a CGM measures glucose in interstitial fluid (a fluid just below the surface of the skin). As glucose levels rise or drop, blood glucose will change slightly quicker than glucose in the interstitial fluid (around 5 to 10 minutes). Therefore, CGM readings are representative of blood glucose 5 to 10 minutes in the past.
- Hand cleanliness: Many inaccurate BGM values are caused by hands not being clean. Wash hands with soap and water (and dry them) right before testing.
- Sensor’s first day: The difference between BGM and CGM readings may be greater with a new sensor. Generally, the readings get closer over the first 24 hours.
- Pressure on your CGM sensor: When something is pressing on the sensor, it can affect your readings. This can be common with side sleepers. Relieve the pressure and the BGM and CGM readings should get closer.
- Rapid glucose change: It can be tricky to compare BGM and CGM readings when glucose is changing quickly, since blood glucose changes before interstitial fluid glucose does. The match should get closer when glucose stabilizes.
- Test strips: If test strips aren’t stored properly or are expired, they may not work correctly. Make sure test strips are stored as directed and not expired. It is also crucial to use enough blood when testing.
The choice between blood glucose monitoring and continuous glucose monitoring depends on individual preferences, lifestyle, and budget considerations. While BGM is common and widely available, the precision and real-time insights offered by CGM can significantly enhance diabetes management, empowering individuals to make informed decisions for insulin treatment decisions. As technology advances, the landscape of glucose monitoring continues to evolve, promising even greater accuracy and convenience in the years to come.