Note for Healthcare Professionals:
Have you recently diagnosed or treated a patient with developmental delay or several delays? As part of a treatment plan, you may be asking your patient’s caregivers to closely monitor the child’s nutrition intake. Below is an explanation of what to expect, geared towards families of a newly-diagnosed child.
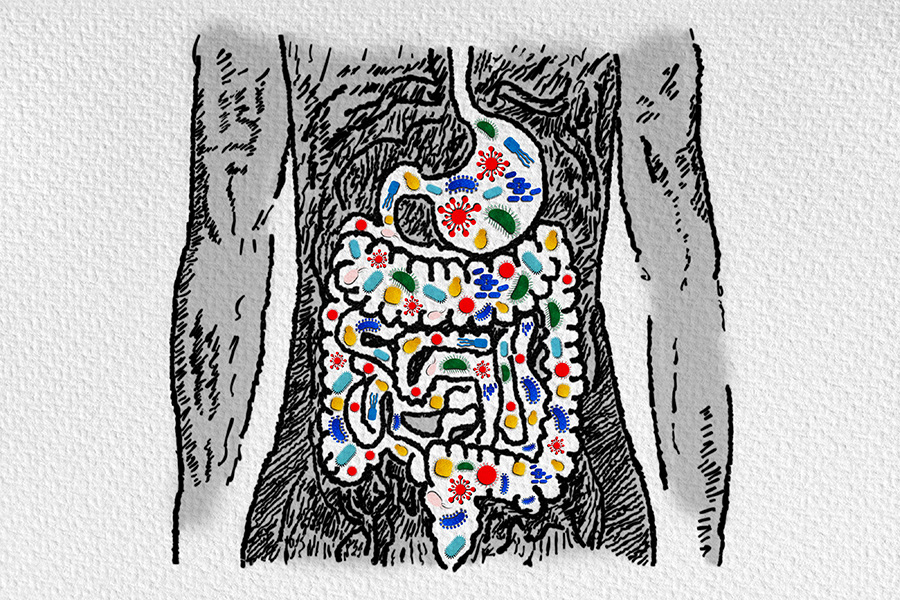
You have recently been told that your child has a developmental delay or several delays. In addition to navigating a wide array of emotions that may surface after hearing your child’s diagnosis, you may also need to be vigilant about your child’s nutrition. There are a few nutritional risk factors for children with developmental delays that caregivers and doctors may be on the lookout for. These often include gastrointestinal disorders, metabolic problems, and feeding issues which can lead to slowed growth in height, obesity, or failure to thrive. Nutritional interventions can be an important step on the path to your child’s development.
How Does Nutrition Impact My Child with Developmental Delay?
Primary nutritional considerations for a child with developmental delays include assessing your child’s growth and evaluating any problems surrounding their energy balance. Secondary major considerations include oral motor problems, developmental delays of feeding skills, inability to self-feed, behavioral problems, and tube feedings. Other areas that may affect their overall nutrition include drug-nutrient interaction, constipation, dental caries (dental cavities or tooth decay), and allergies.
Energy needs for each child with developmental delays vary, just as they do for typical children. A decreased energy need is most apparent with conditions that bring limited gross motor activity or low muscle tone such as Down’s syndrome, spina bifida, Prader-Willi and Turner’s syndrome. Children with cerebral palsy often tend to be seriously underweight for height, and their energy needs are higher than for typical children.
If nutritional problems are identified for your child, their doctor may suggest various types of intervention programs. An interdisciplinary team approach to nutrition management – with the physician, physical therapist, occupational therapist, social worker, nurse, and dietitian all providing input – is key. A unified healthcare team, including all of your child’s caregivers, is an important part of successful nutrition intervention.
When Can I Begin Weaning?
If your child is tube-fed-dependent, you may be anxious to know when you can begin weaning to food taken by mouth. When your child’s medical condition allows for normal oral consumption, weaning from tube feeding can be initiated. This transition over to oral feedings is multifaceted and involves the medical team, your child, and all of your child’s caregivers. Complete weaning from tube feeding should not be considered until your child has achieved a satisfactory nutritional status as your child may stop gaining weight for a time during the transition. Weaning time can vary from a few days to several months. Detailed records of your child’s oral intake should be kept during this time because it is important to maintain adequate nutrition. Tube feedings should be continued until it becomes clear that your child’s nutrient requirements can be met consistently by oral intake over a predetermined period of time.
Oral Aversions
Infant and toddler feeding disorders constitute a tube feeding complication that is unique to young children (the pediatric population.) Many times, when a chronically ill young child is medically ready to begin oral feeding, the infant or toddler may display no interest in eating or may respond with actual hysteria when food, liquid, or utensils are near their face. In this situation, the child typically refuses, cries, gags, or vomits when offered feedings. This oral aversion can occur in children with or without mechanical eating problems.
Due to the emotional component of eating/feeding, a dysfunctional or uninformed caregiver or family member may further the trauma of eating by force feeding or by creating a stressful environment at mealtimes. Children who have been tube fed often do not have normal hunger cycles, normal eating experiences at a table, or a mealtime routine. All these points should be addressed by your healthcare team when the transition to oral feeding begins. Severe cases of oral aversion require intervention and behavior modification from healthcare professionals such as speech pathologists, occupational therapists, and dietitians. This process can be painfully slow.
Initiating oral feedings as soon as medically possible can minimize feeding disorders in some cases. Feeding therapy even when the child is tube-fed-dependent can help alleviate oral aversion. Nonnutritive sucking during tube feedings in infancy can help stimulate oral sucking and swallowing behavior. Positive caregiver-child mealtime interactions are critical for achieving feeding success.
Bonding During Meal Times
Even if your child struggles in some areas of development or is not able to participate in bottle feeding or mealtime like you envisioned, it is important to bond with your child during meal times early on. Hold them during tube feedings, maintain good eye contact, talk to them in a calming tone, laugh and play with them just as you would with an orally-feeding or typically-functioning child. Every child is on their own journey at their own pace, and part of their healthy development is to build a positive relationship with food.
Free Tube Feeding Guides
We are pleased to offer our Adult and Pediatric Tube Feeding Guides for free. These guides provide comprehensive information about tube feeding, including how to care for your tube and the skin around it, how to deliver feedings and how to prevent common complications. This information does not replace the advice of your healthcare professionals.
Request your free copy now!
Bonding with Your Tube Fed Baby
Four Strategies to Bond with Your Baby While Tube Feeding
Getting the news that you cannot breast or bottle feed your child can be difficult to hear. It can make you feel lonely, worried, and heartbroken. But even though you may not be able to nourish your child as you planned…
Click here for the full article.
A Mother’s Perspective: Bonding With Your Tube Fed Child
Julie Bombacino, CEO and co-founder of Real Food Blends, discovered her passion and new career path after learning her child needed a gastrostomy tube. While working through the initial shock and becoming acclimated to their new way of feeding…
Click here to read more.
Tube Feeding Finally Made Food Fun
Three days after my son, Charlie, began tube feeding, we fled to the beach. The ocean in October was exactly what we needed after seven months of fighting to eat…
Click here to continue reading.