You know that feeling when you get home, put the key in the door, and you get that sudden urge to urinate? You squeeze, tell yourself to hold it, cross your legs tightly, run to the toilet and _____. You fill in the blank. This phenomenon is commonly referred to as “The Key in the Door Syndrome” by those who work in the world of urology. This phenomenon, experienced by many women and men, is a symptom of incontinence. (Yes, leaking even a little urine is urinary incontinence.) Nobody wants to be incontinent, but it is a fact among 25 million Americans today. And while incontinence is well-managed through a variety of absorbent products, it is NOT simply an inevitable aspect of aging!
Two types of incontinence that may cause this “Key in the Door” phenomenon are urge incontinence and stress incontinence.
What is Urge Incontinence?
 Urge incontinence occurs when you have a strong and very sudden need to urinate that is difficult to delay. Your bladder squeezes, or spasms, and you lose urine regardless of whether you make it to the bathroom on time. To explain this physiologically, let’s look at how a healthy bladder functions.
Urge incontinence occurs when you have a strong and very sudden need to urinate that is difficult to delay. Your bladder squeezes, or spasms, and you lose urine regardless of whether you make it to the bathroom on time. To explain this physiologically, let’s look at how a healthy bladder functions.
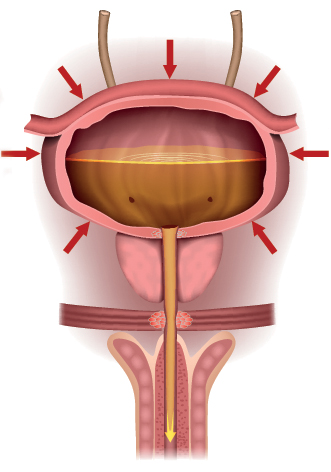
In a healthy bladder, several muscles and body systems work in coordination to control urination. The bladder wall is a muscle that relaxes and expands to hold urine. The sphincter is a muscle around the opening of the bladder. It’s the gateway between your bladder and your urethra: the tube that conveys urine outside your body. Your bladder, which normally can hold more than two cups of urine, will signal via nerves when it is approximately half full (a bit less than one cup). This is the first “urge” to urinate. To control the flow of urine, your bladder wall muscle contracts – or squeezes – to push urine out of the bladder. Simultaneously your sphincter muscle must relax to allow urine to pass through. And systemically, you must also be able to feel and respond to the nerves which convey the urge to urinate.
With urge incontinence, you leak urine because the bladder muscles squeeze – or contract – at the wrong times. These contractions can occur no matter how much urine is in the bladder.
What is Stress Incontinence?
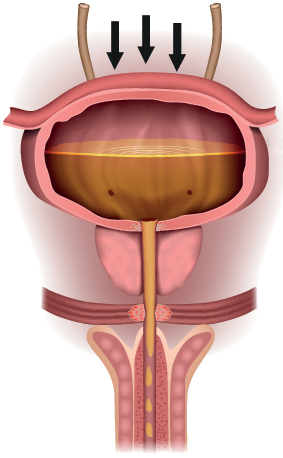 Stress urinary incontinence occurs when your bladder leaks urine during physical activity or exertion. It may happen when you cough, sneeze, lift something heavy, change positions, or exercise. Stress incontinence occurs when the tissue that supports your urethra gets weak.
Stress urinary incontinence occurs when your bladder leaks urine during physical activity or exertion. It may happen when you cough, sneeze, lift something heavy, change positions, or exercise. Stress incontinence occurs when the tissue that supports your urethra gets weak.
We learned above how a healthy bladder works. With stress incontinence, we’re going to focus on the pelvic floor. The pelvic floor is a set of muscles, shaped like a small muscle “hammock,” that runs between the pubic bone in the front and the tailbone at the back. Your bladder, bowel and urethra are supported by your pelvic floor muscles (in women, the uterus is supported by the pelvic floor as well). Your pelvic floor muscles also support the urethra and anus, which pass through them on their way to exit the body. Urine flows from your bladder through your urethra to the outside. When your pelvic floor muscles become weak, urine can slip through when pressure is placed on your bladder. But let’s not forget the sphincter – that muscle around the opening of the bladder. It squeezes to prevent urine from leaking through the urethra. Stress incontinence can happen when your sphincter becomes weak as well.
Is Incontinence Treatable?
There are many factors – such as menopause, obstructions, neurological disorders and more – that contribute to incontinence. Women who have been pregnant (and/or have had a vaginal birth delivery) have experienced stretching every which way imaginable, which contributes to muscle weakness and damage. Men often have incontinence from prostate problems or surgery. All these matters should be discussed and evaluated by your physician to determine the cause of your incontinence.
Although there are many causes of incontinence, we all have pelvic floor muscles (PFM) that strengthen and support our urinary tract, which can help reduce incontinence episodes. We exercise at the gym and workout our skeletal muscles doing things such as bicep curls, squats, and sit-ups. So, why aren’t we regularly exercising our pelvic floor muscles also?
Kegel exercises are well known as the primary exercise to strengthen and tone your pelvic floor muscles. But let’s face it: it’s hard to exercise muscles you cannot see. (Have you seen your pubococcygeus, iliococcygeus, coccygeus or puborectalis? And oh yes, your sphincter too!) If you are currently doing Kegels and are not sure if you are doing them correctly, consider asking your doctor about biofeedback. Physical therapists can teach you how to do Kegel exercises with a technique called biofeedback. This kind of physical therapy may include disrobing from the bottom down, and having sensors or probes placed on your anus and vagina to detect and measure movement. While this is an effective technique, it can also be quite uncomfortable for some people.
Biofeedback at Home
If seeing a physical therapist is not your preference, biofeedback is also possible through Kegel exercise devices that can be used in the privacy of your home. These devices typically include a small, phallic shaped probe that is inserted into the vagina or anus. The probe measures the strength and duration of your pelvic floor muscle (PFM) contractions. This information is then relayed to a small handheld computer, or to an app on your smart phone, so you can visualize the intensity of your muscle strength and the duration. These devices are designed to treat mild-to-moderate urge, stress, and mixed urinary incontinence (mixed urinary incontinence is a combination of urge and stress incontinence) by strengthening the pelvic floor muscles through Kegel exercises. Some apps coach you and provide biofeedback, and some have games to make it more fun. Some of the products are even FDA-approved and reimbursable under Medicare and insurance with a physician’s prescription.
Vaginal weights and electrical stimulation are two other products that you can use at home. Vaginal weights are small, egg-shaped devices that are inserted into the vagina and are held in place by squeezing your pelvic muscles. Weight is increased as strength is gained. Electrical stimulation comes in two types: internal (vaginal) and external. The device automatically stimulates the muscles and does the Kegel exercises for you. Men and women can use external pads to stimulate the muscles through the skin. External devices are an option for those who have an aversion to inserting objects into their body. In some cases, electrical stimulation may also be FDA-approved for stress incontinence.
Why Pelvic Floor Maintenance Is Important
It is so very important to maintain urinary continence throughout our lifetime. Incontinence is one of the primary reasons people go into nursing homes. We walk and do aerobic exercises for our hearts, use weights to prevent osteoporosis – we even do brain exercises to keep our minds sharp as we age. Isn’t it time to start exercising our pelvic floor muscles on a regular basis? Strong pelvic floor muscles not only impact our urinary continence, they also can improve intimacy. Some women claim they have more intense orgasms when their pelvic muscles are stronger. Remember: for Kegels to be effective, you must be dedicated to an ongoing exercise program. Improvements are usually seen in 90 days or less. It takes time and practice to learn how to use any biofeedback devices, so allow yourself time for that learning curve. Maintaining pelvic muscle strength should then become a routine part of your exercise regimen.
So, get the key out of the door, talk to your doctor about urinary leakage, and see if a pelvic floor exercise regimen could help you regain control! Check out the National Association For Continence www.nafc.org for more information, as this is just one component of a continence program.
Sources: