What is Malnutrition and Why Does It Matter?
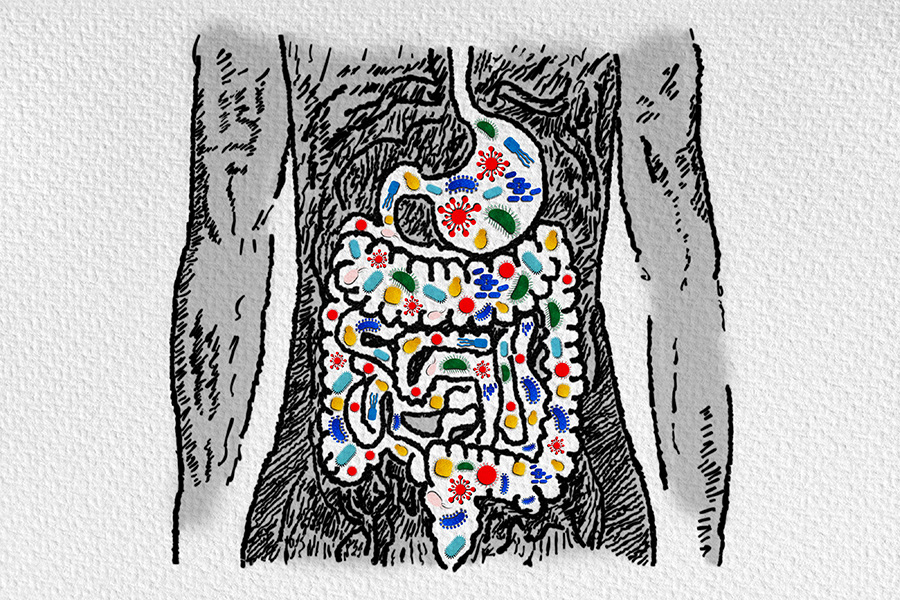
Malnutrition is the condition that occurs when the body is denied vitamins, minerals, and other nutrients it needs to maintain healthy tissues and organ function. When our bodies do not get the right balance of energy and nutrients that it needs, you may become malnourished.
Most people think of undernutrition as the cause of malnutrition. However, malnutrition can also occur with overnutrition, as a result of consuming unbalanced food sources and either too many – or not enough – of certain macro/micronutrients.
Malnutrition threatens your health and your ability to fight sickness and injuries, and it can impact health outcomes from injury or other underlying conditions.
There are four major types of malnutrition:
- Wasting. Defined as low weight-for-height, wasting often indicates recent and severe weight loss. It usually occurs when a person has not had enough food, or enough quality food, and/or they have had frequent or prolonged illnesses.
- Stunting. Defined as low height-for-age, stunting is the result of chronic or recurrent undernutrition. It is usually associated with poverty, poor maternal health and nutrition, frequent illness, and/or inappropriate feeding and care in early life.
- Being underweight. Underweight is defined as low weight-for-age. A person who is underweight may be stunted, wasted, or both.
- Deficiencies in vitamins and minerals. Nutrient deficiencies are a lack of vitamins and minerals that are essential for body functions such as producing enzymes, hormones and other substances needed for growth and development.
How Can We Prevent Malnutrition?
There are three important steps to preventing malnutrition: 1. Nutrition education, 2. Early detection and intervention, and 3. Nutrition supplementation. Depending on a person’s individual situation, any or all of the methods below can help prevent malnutrition.
1. Nutrition education
Whether you are nourishing yourself, a dependent, or you are simply concerned about a loved one, nutrition education is the cornerstone of malnutrition prevention. Valuable topics to educate yourself about include:
- The nutritional value of the most commonly-available foods (see the colorful plate spotlight below!)
- The importance of nutrition in wound healing, and why your body needs more of certain types of nutrients to recover.
- Nutrition both during and after illness, and how it affects recovery.
- The critical importance of sanitary food practices.
- The importance of breastfeeding for an infant’s first six months and continuing to breast feed up to two years or beyond.
- The nutritional advantages of growing a home garden.
Nutrition Education Tip: the Colorful Plate
As a general rule of thumb, the greater the range of colors on your plate, the greater your nutrient diversity. An easy way to make sure that you’re eating a nutrient-rich meal is simply to look at how many different colors your food represents. Food color is nature’s way of hinting what’s inside. When it comes to fruits and vegetables, each color of food contains a unique set of phytochemicals and a unique set of benefits:
- Red: Red fruits and veggies like tomatoes, radishes, strawberries and cherries help support the brain and circulatory system and keep cholesterol levels healthy.
- Orange, Yellow: Carrots, sweet potatoes, peaches, and pineapple provide an instant immunity boost, plus some extra protection for your eyes and bones.
- Green: Green helps with digestion and reduced inflammation. Eat veggies like broccoli, spinach, and brussel sprouts, and choose fruit like kiwi, lime, or green apples.
- Purple, Blue: Eggplant, purple cabbage, blackberries and blueberries can help lower the risk of cancer, heart disease, and stroke. Purple and blue foods have also been linked to improved memory and healthy aging.
- White: White foods like potatoes, cauliflower, bananas and white peaches to help lower bad cholesterol and high blood pressure as well as minimize the risk of certain cancers.
2. Early Detection of Malnutrition and Intervention
For those who are pregnant, infants, and children, the impact of early malnutrition can have lifelong consequences. The longer the growth delays remain uncorrected, the greater the chance of permanent effects. Nutrition interventions are more effective when taking place during pregnancy and first three years of life. A well-recorded growth chart can detect malnutrition very early and is one benefit of regular wellness checks for a growing child. If growth of the child is slowed or arrested, the child’s physician should be alerted, and any hidden infection or reason for nutritional deficiency should be evaluated.
If a child is not receiving regular wellness checks, measurements such as weight, height, mid-arm circumference and chest circumference can be measured and used for nutrition evaluation. The speed of a child’s growth is more important than the actual weight at any given time.
Intervention Tip: Feed Children More Frequently During Illness
Nutritious foods and liquids given frequently, both during and after illness, are necessary for recovery. During an illness, children need additional fluids and encouragement to eat regular meals, and breastfeeding/bottle-fed infants need to breastfeed more often. With some illnesses, dehydration can be a serious risk. A sick child loses a lot of body fluids through increased body temperature, sweating, and sometimes diarrhea. Sick children may have a poor appetite, so offer them nutritious foods in small quantities, and give them fluids frequently – including breastmilk or formula – to help encourage a faster recovery. After an illness, children need to be offered more food than usual to replenish the energy and nourishment lost due to the illness.
3. Nutrition supplementation
Nutrition supplementation can make a critical difference in birth defect prevention, meeting developmental milestones, surgery or injury recovery, and disease treatment and prevention. Biologically vulnerable groups include pregnant women; infants and young children; older adults; and individuals with various health conditions and physical or developmental disabilities which impact their ability to consume a nutrient-rich diet.
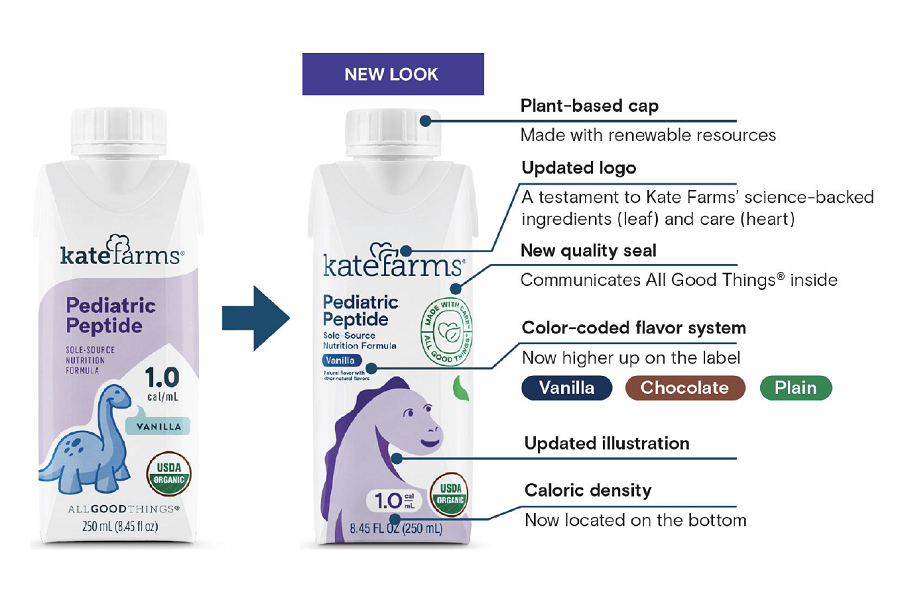
Nutrition Supplementation Tip: Shake It Up With Oral Nutrition Supplements (ONS)
Oral nutrition supplements (ONS), such as a ready-to-drink meal shake, provide additional nutrients – including protein and energy – for people who are not meeting their nutrition needs through food alone. This may be due to poor appetite, reduced food intake, increase in nutrition needs, or poor absorption of nutrients due to illness. ONS are typically used in addition to your usual diet, however some ONS can be used to provide all your nutrition needs for the day if required. ONS are available as ready-to-drink liquids (milk-style or juice-style), powder to add to meals, or dessert-style puddings. While many oral nutrition supplements are available over the counter, your physician or registered dietitian might also prescribe these to you to meet your custom nutritional needs.
How to Spot Malnourishment Symptoms
Below are tips to help individuals and caregivers identify the signs of potential malnutrition.
What To Watch For
Malnutrition may not be immediately apparent. You can help to spot the symptoms by paying attention to changes in:
- Appetite
- How much food you eat
- Bowel habits
- Weight
- Daily activity levels
- Swelling in belly, legs, ankles and feet
If you or your loved one feel well, are eating three meals a day, and have a consistent energy level that allows you to engage in life normally and do what you want to do, then malnutrition is a lower risk.
When To Be Concerned
If you notice any of the following warning signs, discuss them with your healthcare provider:
- Sudden loss or decrease in appetite
- Eating less than 75% of a normal meal for more than a week
- Episodes of nausea, vomiting, or diarrhea for more than three days
- Unplanned weight loss greater than 10 pounds
- Decreased activity level
When You Are in Danger of Malnutrition
The following are dangerous signs that you could be malnourished:
- Eating half as much as you normally do for more than a week
- Persisten nausea, vomiting, or diarrhea
- Sudden and rapid weight loss with noticeable muscle and/or fat loss
- Swelling in feet, ankles, legs or belly
- Feeling confused or having increased memory loss
To learn more, and for resources for individuals, caregivers, and healthcare professionals, visit ASPEN’s Malnutrition Solution Center.