Malnutrition is a critical health issue when a person’s diet lacks essential nutrients, including vitamins, minerals, and proteins. This can lead to numerous health problems and complications if not addressed promptly. By understanding the contributing factors and implementing suitable interventions, we can significantly improve the quality of life for those affected.
Malnutrition Overview
Malnutrition is the condition that occurs when the body is denied vitamins, minerals, and other nutrients it needs to maintain healthy tissues and organ function. When our bodies do not get the right balance of energy and nutrients that they need, we may become malnourished.
There are four major types of malnutrition:
- Wasting. Defined as low weight-for-height, wasting often indicates recent and severe weight loss. It usually occurs when a person has not had enough food, or enough quality food, and/or they have had frequent or prolonged illnesses.
- Stunting. Defined as low height-for-age, stunting is the result of chronic or recurrent undernutrition. It is usually associated with poverty, poor maternal health and nutrition, frequent illness, and/or inappropriate feeding and care in early life.
- Being underweight. Underweight is defined as low weight-for-age. A person who is underweight may be stunted, wasted, or both.
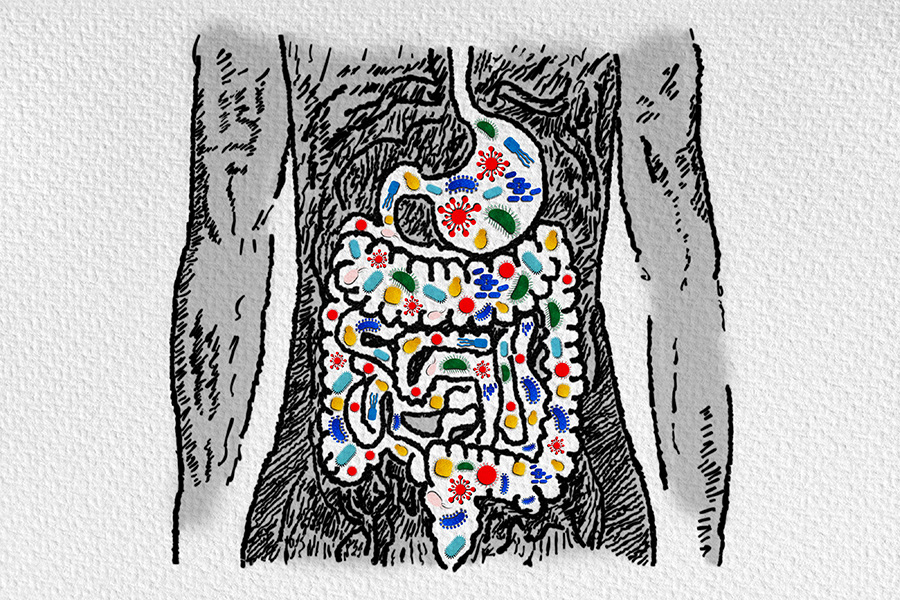
- Deficiencies in vitamins and minerals. Nutrient deficiencies are a lack of vitamins and minerals that are essential for body functions such as producing enzymes, hormones, and other substances needed for growth and development.
Malnutrition Symptoms
Common symptoms of malnutrition include:
- Unintentional weight loss
- Fatigue
- Dizziness
- Frequent infections
- Slow wound healing
- Muscle weakness
These symptoms can vary based on the severity and duration of malnutrition.
The effects of malnutrition on the body can be severe and long-lasting, leading to weakened immune function, impaired cognitive function, and increased susceptibility to infections and chronic diseases. In children, malnutrition can also cause stunted growth and delayed development.
Diagnosis and Tests
Diagnosing malnutrition involves various methods and assessments to determine an individual’s nutritional status. Common techniques used in diagnosing malnutrition include:
- Physical examination: A healthcare professional assesses the patient’s physical appearance, muscle wasting, and signs of nutritional deficiencies.
- Dietary assessment: Evaluating the patient’s dietary intake helps identify any deficiencies or inadequate nutrient consumption.
- Anthropometric measurements: Measurements such as height, weight, and body mass index (BMI) are taken to assess the patient’s nutritional status.
- Subjective global assessment (SGA): A subjective evaluation by a healthcare professional to determine the patient’s overall nutritional status.
- Bone density scan: Measures bone density to identify signs of osteoporosis or low bone mass, which can be related to malnutrition.
- Blood testing:
- Biochemical tests: These measure nutrient levels in the body, such as albumin, prealbumin, and total protein.
- Electrolyte panel: This assesses levels of essential minerals and electrolytes in the body, which can be affected by malnutrition.
- Complete blood count (CBC): This evaluates the number and types of blood cells, providing information about overall health and potential nutrient deficiencies.
If you suspect malnutrition or have concerns about your nutritional status, consult a healthcare professional who can guide you through the diagnosis process and recommend appropriate interventions.
Management and Treatment
Managing and treating malnutrition involves several important interventions to improve nutritional status and overall health. Key strategies include:
- Meal planning: This involves designing meals rich in calories, proteins, and other essential nutrients while considering the individual’s dietary requirements, food preferences, and underlying health conditions.
- Medications and supplements: In some cases, medications or supplements may be prescribed to address specific deficiencies or underlying medical conditions.
- Increasing intake: Adding higher-calorie ingredients and/or snacks into the diet.
- Feeding tube: If you are not able to intake enough nutrition by mouth, you may require a feeding tube. These treatments are usually started in hospital, but they can be continued at home.
- At-home services: Some people who are malnourished need extra care to help them cope with underlying issues such as limited mobility. At-home services, such as Meals on Wheels can provide home-cooked nutritional meals for individuals who cannot provide this for themselves.
It is important to consult a healthcare professional and a registered dietitian before starting new medications, supplements, or meal plans to ensure they suit the individual’s needs.
Malnutrition can have serious long-term effects on health and well-being. Inadequate nutrient intake can lead to various health complications. Recovery and prognosis for malnourished individuals depend on factors such as the severity and duration of malnutrition, underlying health conditions, and access to proper care. With appropriate intervention, such as a balanced diet, nutritional supplements, and medical supervision, many individuals can experience significant health improvements.
However, some long-term effects of malnutrition may be irreversible, particularly if it occurs during critical growth and development periods, impacting physical and mental health. Ongoing care and monitoring are crucial for malnourished individuals. Regular checkups with healthcare professionals ensure nutritional needs are met and potential complications are addressed promptly.
For more malnutrition-related resources, you can visit the Malnutrition Solutions Center hosted by ASPEN, the American Society for Parenteral and Enteral Nutrition.
Keep reading to learn more about nutrition:





















Thank you very much for sharing good information