Only 251 U.S. hospitals receive top ranking on patient experience
Just 251 U.S. hospitals got the highest score on a new five-star rating system the CMS rolled out Thursday.
The new ratings are part of a broader initiative by the federal agency to use a five-star rating system across all of its Web pages intended to help consumers compare the quality of healthcare providers.
Hospitals had a chance to preview the ratings last fall and many have already expressed concern. They question the methodology and whether the ratings reflect “meaningful reflections of performance.” They also say trying to boil down a hospital’s performance to a single score may oversimplify the information that is most relevant to consumers.
Just over 3,500 U.S. hospitals had a new summary rating applied to their Hospital Compare pages on Thursday. According to a Modern Healthcare review of the data, a total of 101 hospitals received the lowest ranking of one star; 582 received two stars; 1,414 received three stars; 1,205 received four stars; and 251 received the highest ranking of five stars.
The summary rating includes an average of hospitals’ performance on each of the 11 publicly reported measures from the Hospital Consumer Assessment of Healthcare Providers and Systems survey. The HCAHPS survey evaluates patients’ experiences at the facilities.
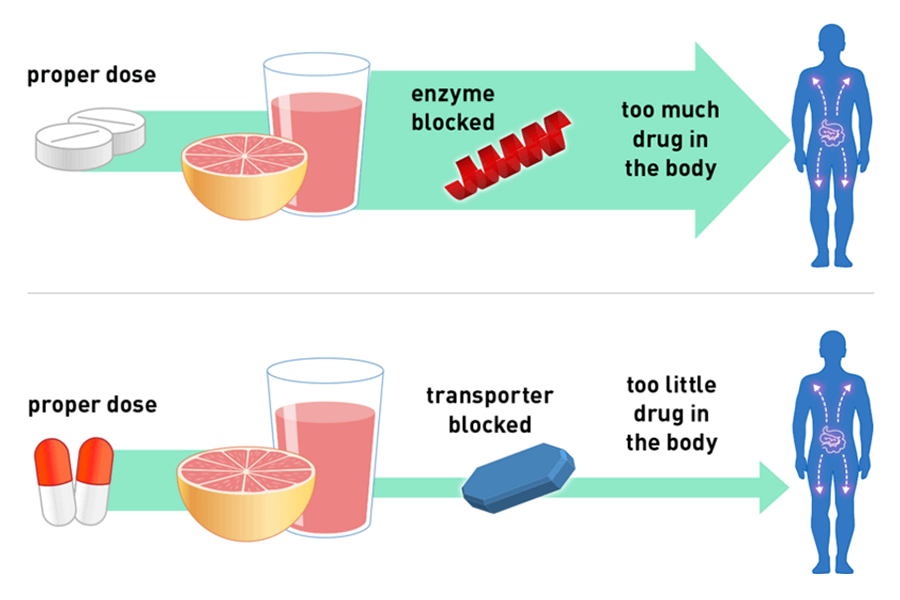
The survey asks patients about factors such as the responsiveness of hospital staff to their needs, the quality of care transitions and how well information about medications is communicated. It also asks about cleanliness and quietness of the facility and whether or not the patient would recommend it to others.
The surveys are provided to a random sampling of patients within two days after they have been discharged from a hospital and must be completed within 42 days. This first round of ratings looks at patient responses gathered between July 1, 2013, and June 30, 2014.
The healthcare industry is under intense pressure to boost the transparency of quality data and provide information consumers can use to make more informed decision about their care. Still, the rollout of CMS’ five-star program on the Compare websites has met with criticism.
The CMS first applied star ratings in 2008 to nursing homes. Last year, the agency rolled out similar programs for home health providers, large group practices and dialysis facilities. The dialysis ratings sparked controversy about the methodology and criticism from the industry that the rating would confuse consumers rather than help them.
Now hospitals are expressing similar concerns.
“The devil is in the details,” wrote the American Hospital Association in an emailed statement. The CMS runs the risk of oversimplifying the complexity of quality care and what is important to a particular patient, the AHA said.
“The reasons that patients seek care from hospitals are varied,” Akin Demehin, the AHA’s senior associate director of policy, said in an interview. “We are not confident that a star-rating approach—especially one that would encompass all of the measures on Hospital Compare and roll them up into a single overall star rating—is going to give patients the insight on the quality of their hospitals that CMS is hoping.”
All three hospitals in the Oregon-based Asante health system received three stars on the new rating. There’s the risk of creating what’s essentially a “black box” for hospitals and consumers, Asante Executive Vice President Scott Kelly said in an interview ahead of the data release.
“The challenge you have with any of these ratings is making sure both consumers and hospitals understand how the ratings are achieved,” Kelly said. “Hospital A is not always comparable to hospital B and C,” he said.
In a news release about Thursday’s release, Dr. Patrick Conway, CMS’ acting principal deputy administrator, said the star ratings encourage hospitals and clinicians to strive to continuously improve the patient experience and quality of care delivered to all patients.
That sentiment was shared by Dr. Penny Wheeler, CEO of Minnesota-based Allina health system. Despite the methodological challenges, she said, “Flawed data is still better than having no data.”
One of Allina’s 12 hospitals received five stars, nine got four stars and two got three stars.
“It’s not perfect; no measurement system is,” Wheeler said. “I don’t know that consumers are making choices based on it, at least not yet. But, it creates a healthy competition among hospitals, which is always good.”
Original article posted by Sabriya Rice of Modern Healthcare on April 16, 2015