Best practices in skin care – including evidence-based measures to prevent, heal and restore skin integrity – are instrumental to improving OASIS outcomes and reducing the financial, clinical and psychological impact of skin breakdown.
The role skin plays in overall health
Intact, healthy skin supports the life of all other body parts. This living barrier is our first line of defense against disease and infection, protecting us from bacteria, dirt and other foreign objects. Skin also protects internal organs from injuries, regulates body temperature and plays an important role in preserving and regulating body fluids.
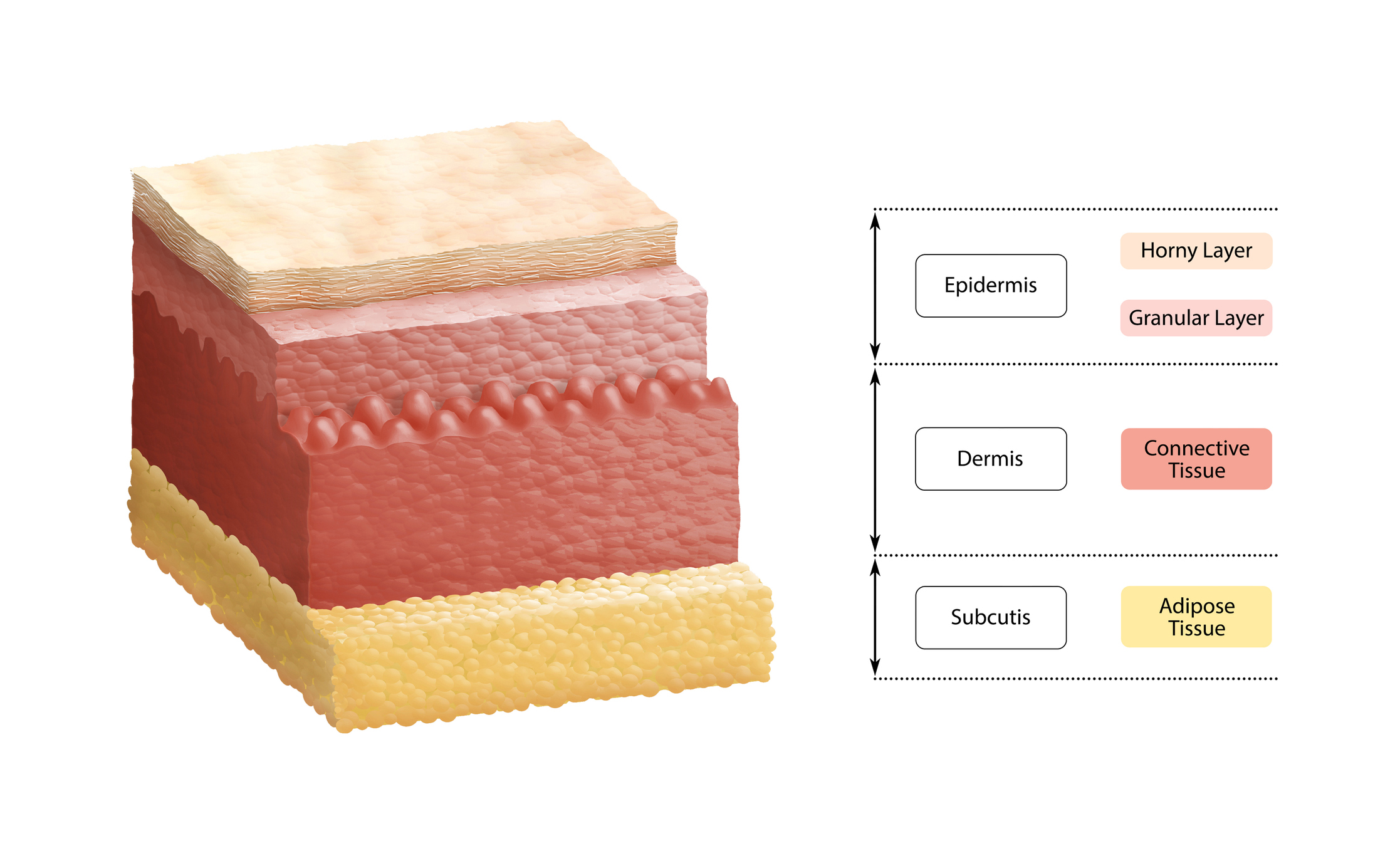
The skin accomplishes all this through its three layers: the epidermis, the dermis, and the hypodermis. The epidermis is the outer layer of the skin, the dermis is in the middle, and the hypodermis is the inner layer of the skin which consists of adipose tissue (fat).
Here are a few vital functions of the layers of the skin:
1. Epidermis
Waterproofing, moisture retention, and serves as a barrier to infection
2. Dermis
Sensation, thermoregulation, tensile strength and elasticity; this layer contains nerve endings, hair follicles, blood vessels, lymphatic vessels, sebaceous (oil) glands and sweat glands
3. Hypodermis (Subcutaneous fat)
Shock absorption, insulation, and attaches the skin to underlying bone and muscle; also the layer where hair follicles are rooted
Who is at risk for skin breakdown?
Poor mobility, certain surgeries, nutrition and hydration issues, advanced age, some medications and certain co-morbidities are all factors that can contribute to skin breakdown. Here are a few examples:
- Individuals with incontinence are susceptible to skin irritation from exposure to urine and stool, leading to incontinence-related dermatitis
- Those who use catheters are at increased risk for urinary tract infections and skin irritation from adhesives or latex
- Someone with a wound often faces a long process of healing, while managing increased risk of infection
- Individuals who receive enteral nutrition (tube-fed) require feeding tube site care and the proper diet to maintain nutrition
- Stoma site care is essential to prevent infections and preserve proper functioning
The consequences of skin breakdown
Quality of Care
Damaged skin can directly impact a person’s satisfaction with quality of care from healthcare professionals. Once the skin is compromised, individuals become susceptible to infection and other potentially life-threatening health complications. Skin breakdown can also affect psychological and emotional well-being, bringing with it pain, depression and reduced mobility. Best practices in skin care can improve overall quality of care by reducing the risk of skin breakdown, reducing pain and infection risk, and improving quality of life for patients, families and caregivers.
Healing Progress
From moisture-associated skin damage to pressure ulcers, skin breakdown can have a profound effect on a person’s healing progress. Pressure ulcers are prevalent, serious medical conditions that can increase morbidity and lengthen hospital stays. Because many pressure ulcers are avoidable, they are now generally considered an important indicator of the person’s quality of care.¹ A good routine based in evidence-backed treatment and preventive care can reduce the risk of complications, and decrease health care costs for both patients and clinicians.
Compensation
Health plans and Medicare are tying more payments to quality of care and patient outcomes. Medicare has not paid for many hospital-acquired conditions since 2008, including catheter-associated urinary tract infections and stage III and IV pressure ulcers. Beginning in FY 2015, the hospital-acquired condition (HAC) reduction program – mandated by the Affordable Care Act – requires the Centers for Medicare & Medicaid Services (CMS) to reduce payments by 1% for hospitals ranked among the lowest-performing 25% in several hospital-acquired conditions.
How The Skin Preservation Program Can Help
Our Skin Preservation resources are designed to educate, inform, and empower patients and health care professionals to identify and resolve challenges addressing skin. From incontinence-associated dermatitis to stoma site infections and pressure ulcers, Shield HealthCare understands that skin issues are complex and affect the overall health and well-being of your patients.
Shield employees have over 1,600 combined hours of specialized wound training from the Wound Care Education Institute®, and more than 100 Certified Wound Management Specialists at Shield HealthCare are available to recommend wound care products on a case-by-case basis.
Learn about our Skin Preservation resources in our Introduction to the Skin Preservation program.
References: