ORIGINAL ARTICLE BY THE DALLAS MORNING NEWS | March 25, 2020
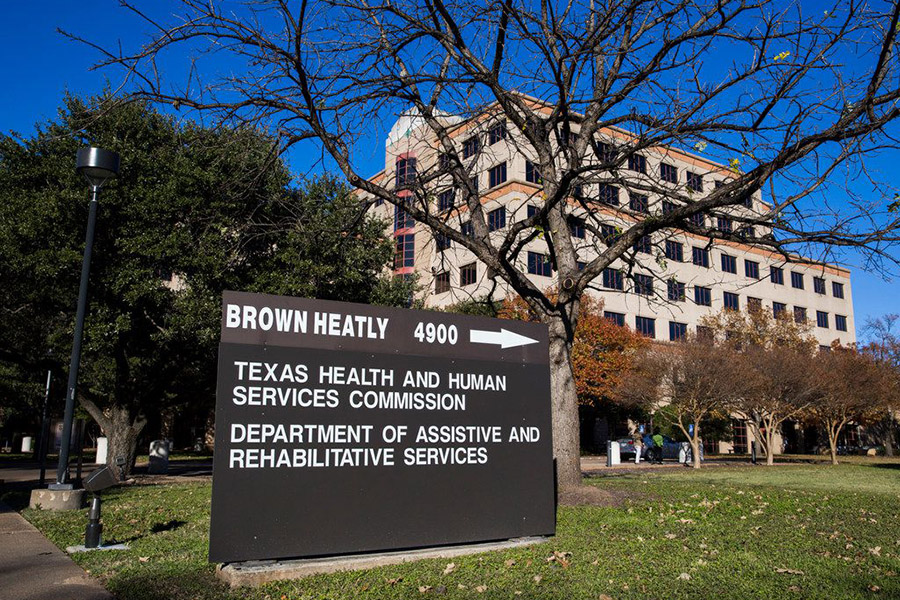
(Above: Bid-scoring irregularities forced the state Medicaid program on Wednesday to scrap managed care contracts for the elderly and disabled, and halt bidding on coverage of children. Bid scorers work for the Texas Health and Human Services Commission, headquartered in north central Austin. – Ashley Landis / Staff Photographer)
Scoring irregularities force the state to scrap managed care contracts for the elderly and disabled, halt bidding on coverage of low-income children, pregnant women and families.
AUSTIN — The state Health and Human Services Commission is canceling $10 billion a year worth of Medicaid managed care contracts for care of the elderly and disabled after again finding discrepancies in its scoring of bids.
On Wednesday, a commission spokeswoman announced that it must scrap contracts awarded in December for STAR+PLUS because of “inconsistent scores by individual evaluators, and outliers in scoring.”
The agency also is halting solicitation of managed care contracts in Medicaid and the Children’s Health Insurance Program, spokeswoman Christine Mann said. Procurement for those two programs is combined, and referred to as STAR CHIP. It offers insurers a book of business that, while consisting of generally healthy people, also is worth about $10 billion a year.
“This decision is necessary to ensure the contract award processes are conducted with integrity, fairness and transparency,” Mann said in a written statement.
In the latest controversy, “multiple” managed care organizations — or MCOs — lodged protests after the commission in October announced winners of STAR+PLUS contracts, Mann said.
Aetna — now part of CVS Health — was one of the big winners, appearing set to become one of three choices of insurance plans that would be given elderly and disabled Medicaid recipients in the service areas around Dallas, Harris, Bexar and Hidalgo counties.
Further review by the commission found scoring irregularities, such as when a bid scorer entered the same response for multiple questions — or when a company’s identical bid for business in different regions received dramatically different ratings.
Though there were wide variations in scoring the same bid, employees didn’t always follow procedures that require for a meeting to discuss why.
Wilson, formerly a top aide to former U.S. Sen. Phil Gramm and former Gov. Rick Perry, runs the Lower Colorado River Authority.
“With such significant concerns raised, it is important to cancel these contracts and ensure our processes result in the best care for our clients at the best value for Texas,” Mann said.
In the past two years, the agency has had two outside firms — Ernst & Young and Mercer — review its contracting procedures. Mercer has urged “better and more consistent training” for bid evaluators and use of a third private contractor to review and manage what happens when the state reposts its solicitations, Mann said.
The decision caps a roller-coaster ride for the MCOs, which assume risk in covering about 4 million low-income Texans. They have grown accustomed to questioning the calls commission procurement staff members make on bids.
In September 2018, a wrangle over insurers’ failures to strictly heed state rules on including historically underutilized businesses caused another postponement — on bidding for both STAR+PLUS and for Medicaid and CHIP.
Last fall, after the commission named tentative winners of STAR+PLUS contracts, two nonprofit insurers that were shut out sued.
Community Health Choice and Community First Health, which grew out of public hospital districts in Houston and San Antonio, respectively, argued that state law gives them a preference. That’s in part because of all the uninsured indigents their public hospitals treat, they argued. Community Health Choice won at the trial court level. The commission is strongly considering an appeal.
CORRECTION: An earlier version of this story misstated the last name of interim Commissioner Phil Wilson