While biofilm may not be at the top of a healthcare professional’s list when she starts wondering why a wound may not be healing – it should be. Biofilm delays healing, and we will explain why below. But let’s start with the what: Biofilm is a community of bacteria. The bacteria attach themselves to the wound, and then cover themselves with a slimy matrix, a sort of a bubble. Unfortunately, antibiotics won’t be able to break through that bubble. The bacteria, under the impenetrable bubble, will start to divide and multiply and will begin to overwhelm the host (the wound).
There are two groups of people out there with houghts about whether or not the human eye can see biofilm: some believe that they can see it, some believe that they can’t. Either way, 60% of chronic wounds have a biofilm.
The problem:
The problem with a wound having a biofilm covering is that it’s going to impede the healing of the wound; it puts a wound into a chronic inflammatory state. This is because the film impairs granulation tissue formation and impairs epithelialization. Biofilm also creates high levels of matrix metalloproteinases (MMPs).
Assessment and diagnosis:
You’ll be able to suspect that a wound has biofilm is by the way the wound behaves: if the wound seems to be healing and then it stalls, if it’s not acting right, then it’s time to consider whether or not it may have a biofilm. But clinically diagnosing biofilm is difficult. There are no specific clinical signs. Traditional lab testing cannot measure bacteria in biofilms. Instead, specialized microscopy is needed (with a confocal laser scanning microscope). Sending it to a specialized lab, however, is not practical in mainstream wound care. Instead, it’s easier to look at the signs and at how the wound behaves. The goal is to reduce and prevent biofilm. Once it’s there, there is no known best method to remove it.
Reduction:
Bacteria harbor in slough. One way to deal with biofilm is to sharp debride – cut it off (if possible, depending on the healthcare professional’s license). Another way is vigorous cleaning: irrigating the wound and getting rid of the surface slough.
Prevention:
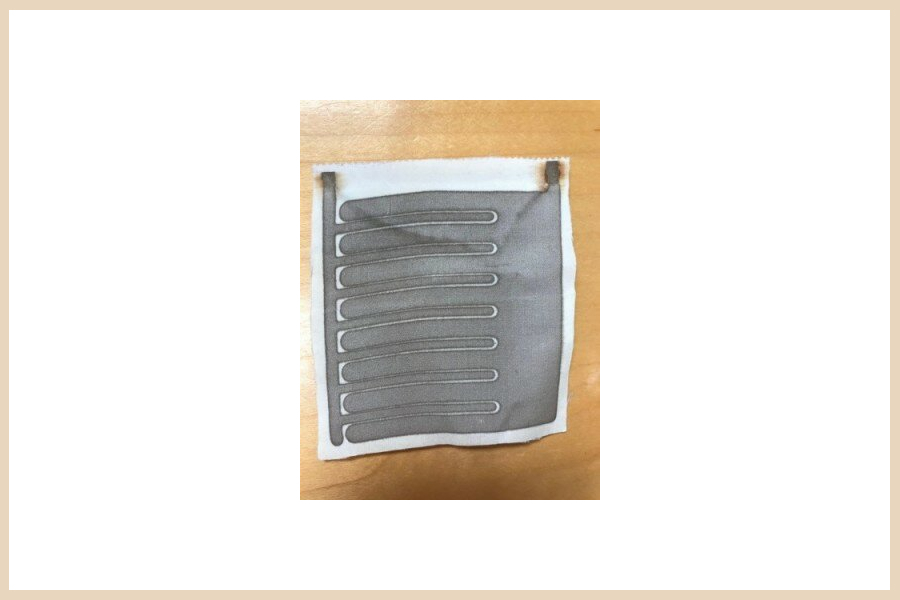
To prevent biofilm from reestablishing, or from occurring in the first place, use products that are broad-spectrum. These will help prevent wound contamination. There are many products out there that are broad-spectrum. One is Silvercel, a silver-based product. Another is a foam, such as Hollister’s Hydrofera Blue READY. These are products that you can put into the wound, and it will help keep out and kill bacteria and decrease the biofilm.
This article was written by a contributing author for Shield HealthCare. This information does not replace the advice of a medical professional. If you have any questions or concerns, please contact your doctor.
Source: The Wound Care Education Institute and our recorded webinar, Is It Infected? How Do I Really Know?
For more information, see related articles and resources here:
- Webinar Video: Is It Infected? How Do I Really Know?
- How Wounds Heal: The 4 Main Phases of Wound Healing
- Video: Pressure Injury Staging Made Easy Recorded Webinar
- Incontinence-Associated Dermatitis: Prevalence, Economic Impact and the Benefits of Prevention
- Pressure Injury Staging: Are You Sure It’s a Pressure Injury?